Medicaid expansion under the Affordable Care Act (ACA) offered the potential to extend health coverage to millions of Americans. But because 23 states opted not to expand Medicaid, 6.3 million uninsured adults have fallen into what’s being called the coverage gap, meaning they earn too much to qualify for Medicaid—but not enough to qualify for Marketplace premium tax credits to help them purchase insurance.
New research from Urban’s Health Policy Center examines the demographic characteristics of the adults who are ineligible for ACA subsidies compared with those who are, and reveals shockingly large disparities involving income, race, gender, and age.
Who falls into the coverage gap? The answer: a very vulnerable segment of the population with very few coverage options and who are likely to remain uninsured. Most of these individuals do not have access to employer-sponsored health insurance, and private coverage is financially beyond their reach.
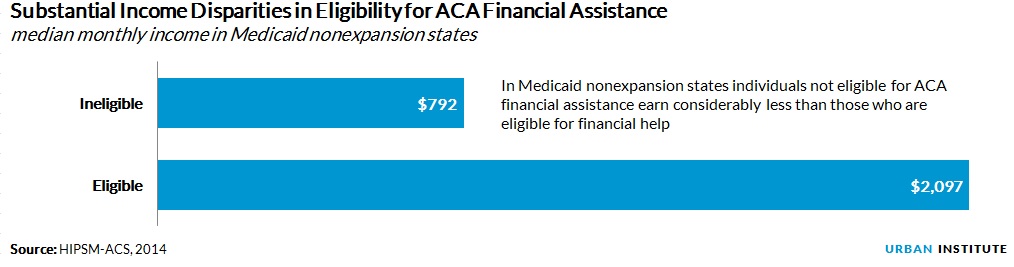
Adults in the coverage gap are significantly poorer compared with those who are eligible for financial assistance. Ineligible adults have a median income of 65 percent of the FPL, while adults who qualify for premium tax credits or subsidies take in 175 percent of the FPL. This is a staggering difference in dollar terms. The median monthly income for those who are ineligible for financial assistance is $792, compared with $2,097 for those who qualify for help.
Because of this significant income gap, uninsured adults’ access to ACA assistance in non-expansion states also varies along racial and ethnic lines. Uninsured black and Latino adults are much more likely to be ineligible for financial help to purchase health insurance than eligible, while white adults are more likely to be eligible for subsidies than ineligible.
Among uninsured black adults, nearly 43 percent (1.6 million people) are ineligible for financial help, and only 28 percent (1 million people) qualify for ACA subsidies.
Adults ineligible for ACA assistance are also more likely to be women, to have no more than a high school education, and to be under age 25.
Despite what the ACA set out to accomplish—filling in the gaps in affordable health coverage for the nation’s poorest residents—states’ decisions not to expand their Medicaid programs are affecting those most in need. As the nation adjusts to the new health reform law, it is important to be mindful of how state policy decisions have created significant disparities in access to care.
Tune in and subscribe today.
The Urban Institute podcast, Evidence in Action, inspires changemakers to lead with evidence and act with equity. Cohosted by Urban President Sarah Rosen Wartell and Executive Vice President Kimberlyn Leary, every episode features in-depth discussions with experts and leaders on topics ranging from how to advance equity, to designing innovative solutions that achieve community impact, to what it means to practice evidence-based leadership.